There is still much to learn about the human microbiome and its role in fighting disease, but ongoing studies at Lawson Health Research Institute, including a focus on fecal microbial transplants (FMT), are making strides in harnessing this complex system.
FMT is being studied in connection with conditions as varied as non-alcoholic fatty liver disease, rheumatoid arthritis, atherosclerosis, HIV, cancer and multiple sclerosis.
FMT is already in clinical use for the treatment of C. diff (Clostridium difficile), and in addition to showing promise in the treatment of other diseases, it is also being studied as a way to improve response to existing cancer treatments and ease treatment side effects.
Dr. Saman Maleki, a Scientist at Lawson Health Research Institute and the London Regional Cancer Program (LRCP) at London Health Sciences Centre (LHSC), says they’ve just begun to explore the possibilities.
"We are just starting to study FMT as an intervention outside its traditional use in patients with C. difficile infection, and we will be expanding to other areas, particularly in cancer.”
FMT can overhaul a patient’s microbiome, Dr. Maleki explains, and a healthy microbiome is beneficial especially when a treatment is trying to activate the body’s immune system.
Dr. Michael Silverman, Lawson Associate Scientist and Medical Director of St. Joseph’s Health Care London’s Infectious Diseases Care Program, is a pioneer in the field of FMT. He has been performing the procedure since 2003 with C. difficile patients and was one of the first in North America to do so. He sees a wide range of possible applications.
“FMT has enormous potential in being an important adjunctive therapy in many cancers. It may, for example, help cancer patients respond to immunotherapy,” says Dr. Silverman, who is also Chair/Chief of Infectious Disease at St. Joseph’s Health Care London, LHSC and Western University. “The potential to impact autoimmune and metabolic diseases is also quite exciting, but still in early development.”
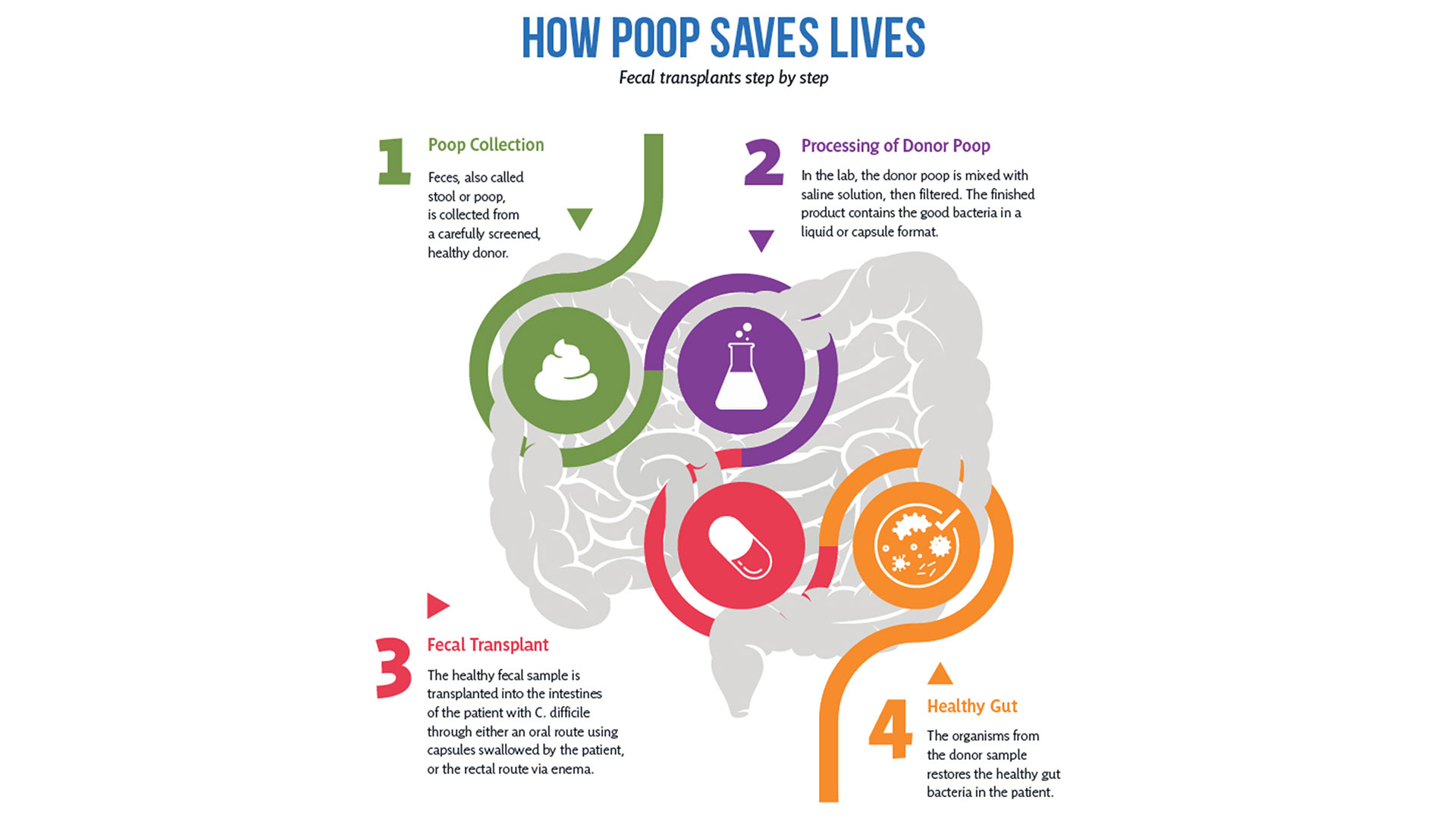
After rigorous screening, stool from a healthy donor is collected and then processed in a lab into a liquid or capsule containing the good bacteria, which can then be administered to a patient’s gastrointestinal tract.
The Lawson team is also one of few delivering FMT using specially-prepared oral capsules. Introduced in 2018, they have been a game changer in patient acceptance and ease of administration, according to Research Coordinator Dr. SeemaNair Parvathy, who has been coordinating the program since 2015.
“There is a link between the fitness of the intestinal microbiome and the fitness of the immune system,” says Dr. John Lenehan, Associate Scientist at Lawson and Medical Oncologist at LHSC. “A ‘healthy’ microbiome leads to a more robust immune response when using immunotherapy. FMT from a healthy donor is expected to improve the fitness of the recipient’s intestinal microbiome and promote a better immune response.”
People with chronic disease can often experience what’s called a ‘leaky gut,’ allowing food, bacterial and microbial components to pass through the intestinal wall, negatively impacting the immune system.
“When people get FMTs their intestinal permeability improves – meaning it actually reduces,” says Dr. Jeremy Burton, Lawson Scientist and Research Chair of Human Microbiome and Probiotics at Lawson and St. Joseph’s. “What changes that intestinal permeability? The microbes at the site. They play a role in interacting with the host cells, providing nutrients and vitamins.”
With the immune system so closely tied to the health of the microbiome, it’s not surprising scientists are exploring how strengthening one can have a big impact on the other.
Immunotherapy can be used to either stimulate or suppress the immune system to help the body fight disease, and FMT is showing promise in reducing resistance to the treatment.
While immunotherapy has been effective in treating a number of cancers – the number one cause of death in Canada – not all patients respond to the treatment.
But early work presented at a conference by the Lawson team for the Journal for ImmunoTherapy of Cancer has shown that using FMT to modify the microbiome could reduce resistance to immunotherapy. The study involved patients from LHSC with advanced melanoma, a type of skin cancer.
While in the very early stages, the combination of FMT and anti-PD1 immunotherapy has been found to be safe, and it appears that FMT could make tumours more responsive to the immunotherapy treatment.
“Microbiome-based treatment strategies, including FMT, have a high potential in oncology,” says Dr. Maleki. “Our team is also exploring its potential in treating pancreatic cancer.”
The research is so interesting that a recent Nature article listed the Phase I melanoma trial as “seminal” research. The study was also unique in that it used healthy donors, as opposed to donors who had previously responded to immunotherapy treatment.
A separate Lawson study with LHSC patients with metastatic renal cell carcinoma, a type of kidney cancer, published in the Journal of Clinical Oncology, also looked at combining immunotherapy and FMT to ease the adverse effects of the treatment.
The Phase I study, led by Dr. Maleki and Dr. Ricardo Fernandes, Medical Oncologist at LHSC, found adding FMT to doublet immunotherapy was safe, but further study is needed to determine whether it could bring about changes in the microbiome and immune system.
Dr. Lenehan says Lawson researchers are in a position to be leaders in this field in the near future for two reasons.
“One is that other academic researchers have not been able to assemble the expertise, and some who have, do not have the access to healthy donor stool. The second is that some biotechnology companies are interested in FMT, but almost exclusively for C. difficile infections.”
Two other areas that have seen recent advances include FMT for the treatment of non-alcoholic fatty liver disease (NAFLD) and multiple sclerosis.
“The gut microbiome is very important in the metabolism of foods and metabolic products. It can therefore have a major effect on obesity and atherosclerosis,” says Dr. Silverman. “It also is tightly involved in regulating the immune system and therefore moderating the microbiome may potentially impact autoimmune diseases.”
A study published in 2020 by the team in The American Journal of Gastroenterology showed that FMT appears to reduce intestinal permeability in patients with NAFLD.
The number of people with NAFLD is growing rapidly and studies show patients have different microbiota than healthy persons.
The trial included 21 NAFLD patients from LHSC and St. Joseph’s. While the researchers found no changes in percentage of liver fat or insulin resistance, they observed significant reduction in intestinal permeability in those patients who had elevated intestinal permeability at the study’s start (seven patients in total). They also observed changes to the gut microbiome in all patients who received a fecal transplant from a healthy donor.
“Metabolic syndromes including obesity and its complications of NAFLD and atherosclerosis are massive public health problems. Any impact on these would be of huge importance,” Dr. Silverman adds. “Autoimmune diseases also cause major morbidity and mortality. We have a lot of work to do before we can consider FMT as a routine therapy for any of these conditions, but the long-term promise is great.”
Research into the use of FMT for treatment of patients with multiple sclerosis is in the very early stages. But patients with MS show a difference in gut microbiota and higher small intestine permeability, which could contribute to the development of the disease.
A Phase I trial by the Lawson team published in the Multiple Sclerosis Journal – Experimental, Translational and Clinical, found FMT to be safe and tolerable.
While the study was very small, MS patients treated with FMT were found to have beneficial changes to gut microbiota and intestinal permeability, but further study is needed to determine if FMT could be used as a treatment.
Lawson scientists are also currently studying the use of FMT for patients with atherosclerosis, along with ongoing studies on melanoma and lung cancer. Funding for a study on pancreatic cancer has been secured and researchers are in the process of planning trials for a number of other applications.
Dr. Lenehan says, “The microbiome is connected to several diseases and their treatments. Evidence is growing that an individual’s health is related to their microbiome.”

The challenge of finding fecal donors for FMT and the cost of that process remain an issue for research into this promising treatment, even as more potential applications are discovered.
There is currently no process in place to match donors and recipients – as with organ donation – but there is an extensive screening process for both infectious and non-infectious conditions, one that needs to be repeated if a donor experiences any lifestyle changes.
Dr. Burton says, “We still don't understand the full role of the microbiota. We have to ensure that we're not giving patients a microbiota that might cause them some other issue in the future, so the donors are screened very thoroughly for that.”
Screening also excludes donors with an increased risk of developing the diseases scientists are hoping to treat, such as metabolic syndrome related conditions.
A 2017 article published in Open Forum Infectious Diseases by Drs. Silverman and Burton found the cost of screening high numbers of potential donors could make establishing local programs extremely difficult, so having a central program such as the one in London could help patients in many regions.
In the study, only five of 46 potential donors passed the history, examination, blood, stool and urine tests, and of the five, four later travelled or had illnesses that made donation inadvisable.
The search continues in London for potential donors to help drive this research forward. You can read one donor’s story and learn how you can get involved here.
More on FMT and the microbiome:
Drugs vs. bugs: Harnessing the microbiome to improve treatments
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email