Additional Research Activities
Transforming growth factor-beta and bone morphogenetic protein signalling: I was the first to discover that ovarian cancer cells possess intact bone morphogenetic protein (BMP) signalling that functions to promote cell spreading via cell-substratum adhesion [Shepherd and Nachtigal (2003) Endocrinology] as well as to upregulate the ID1 and ID3 proto-oncogene overexpression observed in ovarian tumours [Shepherd et al. (2008) Gene]. As an independent investigator, I have extended this work to show that BMP signalling was downregulated during spheroid formation to promote cell aggregation, and that ectopic expression of a constitutively-active BMP type I receptor negatively impacts spheroid formation [Peart et al. (2012) Clin Exp Metastasis].
Tumour spheroids as a model system for discovery research: An essential component of my laboratory’s research was the development and use of an in vitro experimentally-tractable model system that mimics ovarian cancer metastasis. I have developed a rapid, easy and reproducible cell culture system to establish spheroids in liquid suspension, where they can be visualized microscopically, treated with pharmacologic agents or viral vectors, and subsequently transferred to adherent culture as a model of secondary tumour formation.
Oncolytic viruses: A secondary objective for our spheroid culture system of ovarian cancer metastasis, particularly with ascites-derived clinical specimens, is to directly test the efficacy of novel therapeutics.
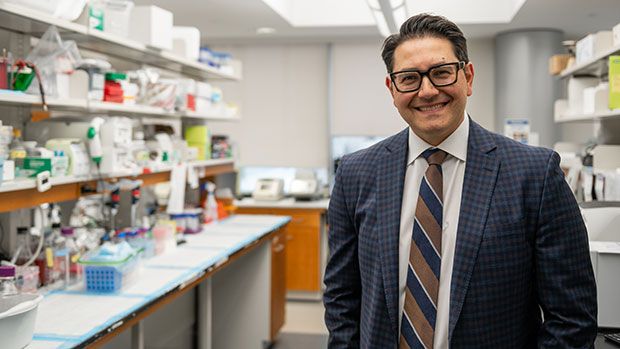
Trevor Shepherd obtained his undergraduate degree from The University of Western Ontario Honours Genetics Program in 1995 before going on to perform graduate studies with Dr. John Hassell at McMaster University. For his PhD, he studied the function of the PEA3 subfamily of Ets transcription factors in breast cancer using transgenic mouse models in collaboration with Dr. Bill Muller. After completing his PhD degree in 2002, he switched to studying ovarian cancer with Dr. Mark Nachtigal at Dalhousie University where he initiated his work with patient-derived primary cell culture techniques. He was recruited back to Southwestern Ontario in 2007 as an Assistant Professor in Ob/Gyn, Oncology and Anatomy & Cell Biology at Western University and a Translational Oncology Scientist at the London Regional Cancer Program. His work over the last several years has focused on developing an in vitro model of ovarian cancer metastasis to investigate altered pathobiology and how these malignant changes can be targeted therapeutically. His work has been supported by the US DOD, CRS, and CCSRI, and he currently holds a CIHR grant to investigate stress metabolism signalling in ovarian cancer metastasis and tumour dormancy.